Treatment of paresis
**- Medical care. **Stroke patients require medical monitoring and care to manage stroke-related complications such as high blood pressure, diabetes, heart disease, etc. Medications such as anticoagulants and antiplatelet drugs can be used to reduce the risk of a recurrence of a stroke.
- Rehabilitation and physiotherapy. Physiotherapy is a crucial element of the treatment of post-stroke paresis. A physical therapist will develop a rehabilitation program that includes exercises to improve muscle strength, balance, coordination, and range of motion. Exercises can be conducted both in a clinical setting and at home.
- Occupational therapy. It focuses on improving functional skills and independent functioning. An occupational therapist can help you regain everyday skills such as eating, dressing, washing, writing, etc., through exercise, training in compensatory techniques, and technical aids.
- Speech therapy. If stroke affects speech and swallowing, speech therapy may be necessary. A speech therapist will help improve pronunciation, understanding, and speech production and rehabilitate swallowing functions.
**- Psychological therapy and support. **Post-stroke paresis can affect the patient's emotional well-being. Psychological therapy, emotional support, and support groups can help deal with emotional difficulties and adapt to change.
- Pharmacological therapy. In some cases, medications may be used to manage accompanying symptoms such as pain, muscle spasms, tremors, etc. Your doctor may prescribe painkillers, muscle relaxants, antihypertensives, etc.
- Surgical interventions. In cases where post-traumatic paresis is significant and significantly limits the patient's functioning, surgical interventions such as drug pump implantation or revascularization surgery may be considered to restore blood flow to the damaged area of the brain.
- Brain Neuromodulation Transcranial Magnetic Stimulation (TMS), a non-invasive neuromodulation technique, uses magnetic pulses to modulate the activity of specific brain regions. This supports functional reorganisation and helps restore motor abilities. As a result, it enables more effective motor recovery and improves patients’ quality of life. TMS therapy is commonly administered on an outpatient basis in Western countries, such as Germany.
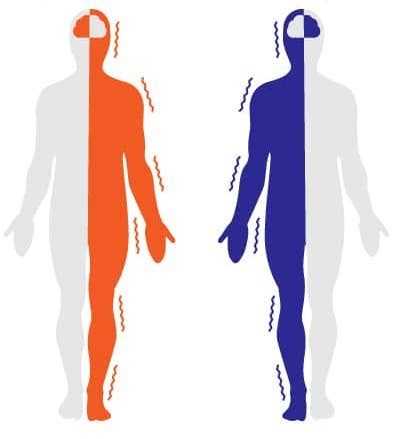
- Peripheral Magnetic Stimulation (mPNS) in Post-Stroke Rehabilitation Peripheral Magnetic Stimulation (mPNS) works by activating nerves and muscles through magnetic pulses, thereby supporting the recovery of motor functions and alleviating pain. This method can be particularly beneficial when traditional rehabilitation approaches are limited due to pain or difficulty initiating voluntary movement.